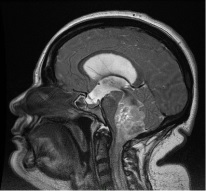
Diagnóstico diferencial de las lesiones del IV ventrículo
DOI:
https://doi.org/10.53903/01212095.17Palabras clave:
Meduloblastoma, Astrocitoma, Ependimoma, HemangioblastomaResumen
La población pediátrica es, de lejos, la más afectada por las lesiones del cuarto (IV) ventrículo. La gran mayoría presentan un patrón radiológico similar; actualmente, con las secuencias de difusión, espectroscopia y mapas de ADC, se puede inferir la compatibilidad de los hallazgos visualizados con alguna de las patologías que se revisarán en el presente trabajo.
Descargas
Referencias bibliográficas
Fontana H, Belziti H, Requejo F, Recchia M. Buratti S. Los recesos del IV ventrículo. Rev Argent Neuroc. 2006; 20:101-13.
Agarwal A, Kanekar S. Intraventricular tumors. Semin Ultrasound CT MRI. 2016;37:150-8.
Koeller K, Sandberg G. Cerebral intraventricular neoplasms: radiologic-pathologic correlation. Radiographics. 2002;(22):1473-505.
Smith A, Simirniotopoulos J. Horkanyne-Szakaly I. Intraventricular Neoplasms: Radiologic- Pathologic Correlation. RadioGraphics. 2013;33:21-43.
Salgado A, Shehadeh S, Morales E, Santamarta E, Morán M, Saiz A, Oviedo E. Lesiones inusuales de la fosa posterior. Hallazgos de Neuroimagen. S-1299 SERAM.
Wolff J, Sajedi M, Brant R, Coppes M, Egeler R. Choroid plexus tumours. Br J Cancer. 2002;87:1086-91.
Jusué I, Ortega M, Tamarit M, Poveda P. Papiloma atípico de los plexos coroideos en el adulto: publicación de un caso clínico y revisión de la bibliografía. Neurocirugía. 2012;23(3):116-21.
Louis D, Perry A, Reifenberger G, Von Deimling A, Figarella-Branger D, Cavenee W, et al. The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. Acta Neuropathol. 2016;131:803-20.
Fenchel M, Beschorner R, Naegele T, Korn A, Ernemann U, Hoger M. Primarily solid intraventricular brain tumors. Eur J Radiol. 2012;81:e688-96.
Hernández P, Villanueva M, Vacas M, Sánchez J, Asensio J, Villanueva J. Tumores intraventriculares: Revisión de los hallazgos radiológicos característicos mediante TC y RM convencional. Congreso de la SERAM; 2012, mayo 24-28. Disponible en: https://epos.myesr.org/poster/esr/seram2012/S-1331.
Zabala I, Llorente S, Laganâ C, Barbosa del Olmo A, Cigüenza Sancho M, Gordillo Vélez CH. Tumores intraventriculares: Nuevas entidades y hallazgos recientes en resonancia magnética. Congreso de la SERAM; 2014. Disponible en: https://epos. myesr.org/poster/esr/seram2014/S-0546.
Shih RY, Smirniotopoulos JG. Posterior fossa tumors in adult patients. Neuroimag Clin N Am. 2016;26:493-510.
Bohara M, Baru M, Fujio S, Higashi M, Yonezawa H, Karki P, et al. Choroid plexus tumors: experience of 10 cases with special references to adult cases. Neurol Med Chir. 2015;55:891-900.
Krieger MD, Panigrahy A, McComb JG, Nelson MD, Liu X, González-Gómez I, et al. Differentiation of choroid plexus tumors by advanced magnetic resonance spectroscopy. Neurosurgical focus. 2005;15:18(6A).
Verma A, Kumar I, Verma N, Aggarwal P, Ojha R. Magnetic resonance spectroscopy — Revisiting the biochemical and molecular milieu of brain tumors. BBA Clinical. 2016;5:170-8.
Grossman R, Ram Z. Posterior fossa intra-axial tumors in adults. World Neurosurg. 2016;88:140-5. doi: 10.1016/j.wneu.2015.12.066.
Raynaud C, Ramaswamy V, Taylor M, Laughlin S. Posterior fossa tumors in children: Developmental anatomy and diagnostic imaging. Childs Nerv Syst. 2015;31:1661-76.
Thompson YY, Ramaswamy V, Diamandis P, Daniels C, Taylor MD. Posterior fossa ependymoma: current insights. Childs Nerv Syst. 2015;31:1699-706.
Sayegh ET, Aranda D, Kim JM, Oh T, Parsa AT, Oh MC. Prognosis by tumor location in adults with intracranial ependymomas. J Clin Neurosci. 2014;21(12):2096-101.
U-King-Im JM, Taylor MD, Raybaud C. Posterior fossa ependymomas: new radiological classification with surgical correlation. Childs Nerv Syst. 2010;26:1765-72.
Olabarria IV, Villanúa JA, Fernández B, Ontañon JM, Cabrera A, Saralegui I. Tumores de fosa posterior y Difusión. Congreso Seram. Granada; 24-28 de mayo de 2012. Disponible en: https://epos.myesr.org/poster/esr/seram2012/S-0891.
Brandão LA, Castillo M. Adult brain tumors clinicalapplications of magnetic resonance spectroscopy. Magn Reson Imaging Clin N Am. 2016;24:781-809.
Majós C, Aguilera C, Cos C, Camins À, Candiota AP, Delgado-Goñi T, et al. In vivo proton magnetic resonance spectroscopy of intraventricular tumours of the brain. Eur Radiol. 2009;19:2049-59.
Kim Y, Lee SY, Yi KS, Cha S, Gang M, Cho B, et al. Infratentorial and Intraparenchymal Subependymoma in the Cerebellum: Case Report. Korean J Radiol. 2014;15(1):151-5.
Landriel F, Besada C, Migliaro M, Christiansen S, Goldschmidt E, Yampolsky C, et al. Atypical hemorrhagic presentation of a fourth ventricle subependymoma: Case Report. Neurol Med Chir (Tokyo). 2013;53:828-31.
Jain A, Amin AG, Jain P, Burger P, Jallo GI, Lim M, et al. Subependymoma: clinical features and surgical outcomes. Neurol Res. 2012;34(7):677-84.
Burguete A. WHO grade I intraventricular tumors: findings in diffusion, perfusion and spectroscopy. Congreso SERAM C-1990. Coruña 2012. Disponible en: https:// epos.myesr.org/poster/esr/ecr2012/C-1990.
Ragel BT, Osborn AG, Whang K, Townsend JJ, Jensen RL, Couldwell WT. Subependymomas: An analysis of clinical and imaging features. Neurosurgery. 2006;58:881-90.
Alver I, Abuzayed B, Kafadar AM, Muhammedrezai S, Sanuz GZ, Akar Z. Primary Fourth Ventricular Meningioma: Case Report and Review of the Literature. Turkish Neurosurgery. 2011;21(2):249-253.
Takeuchi S, Sugawara T, Masaoka H, Takasato Y. Fourth ventricular meningioma: a case report and literature review. Acta Neurol Belg. 2012;112:97-100.
Khedr S, Hassaan M, Refaat A. The diagnostic value of diffusion weighted imaging in patients with meningioma. Egyptian J Radiol Nuclear Med. 2012;43:249-56.
Cabada T, Caballero M, Insausti I, Álvarez de Eulate N, Bacaicoa C, Zazpe I, et al. Papel de la difusión en la evaluacion de los meningiomas: correlación radiopatológica. Radiología. 2009;51(4):411-9.
Yin B, Liu L, Zhang B, Li YX, Li Y, et al. Correlating apparent diffusion coefficients with histopathologic findings on meningiomas. Eur J Radiol. 2012;81:4050-6.
Poretti A, Meoded A, Huisman T. Neuroimaging of pediatric posterior fossa tumors including review of the literature. J Magnetic Resonance Imag. 2012;35(1):32-47.
Coyle B, Kessler M, Sabnis D, Kerr I. ABCB1 in children’s brain tumours. Biochem Soc Trans. 2015;43(5):1018-22.
Massimino M, Biassoni V, Gandola L, Garrè M, Gatta G, Giangaspero F, et al. Childhood medulloblastoma. Crit Rev Oncol/Hematol. 2016;105:35-51. http://dx.doi. org/10.1016/j.critrevonc.2016.05.012.
Bartlett F, Kortmann R, Saran F. Medulloblastoma. Clin Oncol. 2013;25(1):36-45. 38. Taylor M, Northcott P, Korshunov A, Remke M, Cho Y, Clifford S, et al. Molecular subgroups of medulloblastoma: the current consensus. Acta Neuropathol. 2012;123(4):465-72.
Northcott P, Korshunov A, Pfister S, Taylor M. The clinical implications of medulloblastoma subgroups. Nat Rev Neurol. 2012;8(6):340-51. doi:10.1038/nrneurol. 2012.78.
Martínez M. Meduloblastoma pediátrico, revisión y puesta al día. Radiología. 2011;53(2):134-45.
Yamashita Y, Kumabe T, Higano S, Watanabe M, Tominaga T. Minimum apparent diffusion coefficient is significantly correlated with cellularity in medulloblastomas. Neurological Research. 2009;31(9):940-6.
Abdul Z, Saini J, Ranjan M, Gupta A, Sabharwal P, Purushotham N. Diffusion tensor imaging in evaluation of posterior fossa tumors in children on a 3T MRI scanner. Indian J Radiol Imaging. 2015;25(4):445-52.
Pierce T, Kranz P, Roth C, Leong D, Wei P, Provenzale J. Use of apparent diffusion coefficient values for diagnosis of pediatric posterior fossa tumors. Neuroradiol J. 2014;27:233-44.
Rodríguez D, Awwad A, Meijer L, Manita M, Jaspan T, Dineen R, et al. Metrics and textural features of MRI diffusion to improve classification of pediatric posterior fossa tumors. Am J Neuroradiol. 2014;35:1009-15.
Rumboldt Z, Camacho D, Lake D, Welsh C, Castillo M. Apparent diffusion coefficients for differentiation of cerebellar tumors in children. Am J Neuroradiol. 2006;27:1362-9.
Jouanneau E, Guzmán R, Desuzinges C, Frappaz D, Louis-Tisserand G, Sunyach MP, et al. Very late frontal relapse of medulloblastoma mimicking a meningioma in an adult: Usefulness of H-Magnetic resonance spectroscopy and diffusion-perfusion magnetic resonance imaging for preoperative diagnosis: case report. Neurosurgery. 2006;58:789-90.
Baker S, Ellison D, Gutmann D. Pediatric gliomas as neurodevelopmental disorders. Glia. 2016;64(6):879-95.
Helfferich J, Nijmeijer R, Brouwer O, Boon M, Fock A, Hoving E, et al. Neurofibromatosis type 1 associated low grade gliomas: A comparison with sporadic low grade gliomas. Critical Rev Oncol/Hematol. 2016;104:30-41.
Arango J, Menor F, Viguer R, Esteban M, Palacios P, Assing O. Astrocitoma pilocítico pediátrico. Aproximación diagnóstica con TC y RM. Congreso de la SERAM 2012. Disponible en: https://epos.myesr.org/poster/esr/seram2012/S-0744.
Gaudio S, Martucci M, Russo R, Visconti E, Gangemi E, D’Argento F, et al. MR imaging of brain pilocytic astrocytoma: beyond the stereotype of benign astrocytoma. Childs Nerv Syst. 2017;33(1):35-54.
Collins V, Jones D, Giannini C. Pilocytic astrocytoma: pathology, molecular mechanisms and markers. Acta Neuropathol. 2015;129:775-88.
Docampo J, González N, Muñoz A, Bruno C, Morales C. Astrocitoma pilocítico. Formas de presentación. Rev Argent Radiol. 2014;78(2):68-81.
Brandão L, Shiroishi M, Law M. A Multimodality approach with diffusion- weighted imaging, diffusion tensor imaging, magnetic resonance spectroscopy, dynamic susceptibility contrast and dynamic contrast-enhanced magnetic resonance imaging. Magn Reson Imaging Clin N Am. 2013;21(2):199-239.
Grand S, Kremer S, Tropres I, Hoffmann D, Chabardes S, Lefournier V, et al. Perfusion-sensitive MRI of pilocytic astrocytomas: initial results. Neuroradiology. 2007;49(7):545-50.
Uematsu H, M Maeda. Double-echo perfusion-weighted MR imaging: basic concepts and application in brain tumors for the assessment of tumor blood volume and vascular permeability. Eur Radiol. 2006;16(1):180-6.
Findeis-Hosey JJ, McMahon KQ, Findeis SK. Von Hippel–Lindau Disease. J Pediatr Genet. 2016;5(2):116-23. http://dx.doi.org/ 10.1055/s-0036-1579757.
Schunemann V, Huntoon K, Lonser RR. Personalized medicine for nervous system manifestations of von Hippel–Lindau Disease. Front Surg. 2016;3:39.
Wang Z, Hu J, Xu L, Malaguit J, Chen S. Intratumoral hemorrhage in a patient with cerebellar hemangioblastoma a case report and review. Medicine (Baltimore). 2015;94(4):e497.
Osorio D, Guevara J. Diagnóstico de hemangioblastoma por tomografía computarizada. Concordancia interobservador. Rev Med IMSS. 2002;40(5):393-7.
Arora R. Imaging spectrum of cerebellar pathologies: A pictorial essay. Pol J Radiol. 2015;80:142-50.
Leung R, Biswas S, Duncan M, Rankin S. Imaging features of von HippelLindau Disease. RadioGraphics. 2008;28:65-79.
Raz E, Zagzag D, Saba L, Mannelli L, Paolo P, Ambrosio F, et al. Cyst with a mural nodule tumor of the brain. Cancer Imaging. 2012;12:237-44.
Guan T, Pancharatnam D, Chandran H, Hooi T, Kumar G, Ganesan D. Infratentorial benign cystic meningioma mimicking a hemangioblastoma radiologically and a pilocytic astrocytoma intraoperatively: a case report. J Medical Case Reports. 2013;7:87.
Cho S, Na D, Ryoo J, Roh H, Moon C, Byun H, et al. Perfusion MR Imaging: Clinical utility for the differential diagnosis of various brain tumors. Korean J Radiol. 2002;3:171-9.
Jensen T, Post J. Intraventricular neurocysticercosis: Presentation, diagnosis and management. Asian Pacific Journal of Tropical Medicine. 2016;9(8):815-8. http:// dx.doi.org/10.1016/ j.apjtm.2016.06.016
Sinha S, Sharma B. Intraventricular neurocysticercosis: a review of current status and management issues. Br J Neurosurg. 2012;26(3):305-9.
Kimura ET, Higuera JA, Corona R, Chávez L, Perochena A, Quiroz L, et al. Neurocysticercosis: Radiologic-Pathologic Correlation. RadioGraphics. 2010;30(6):1705-19.
Sarria S, Frascheri L, Siurana S, Auger C, Rovira A. Neurocisticercosis. Hallazgos radiológicos. Radiología. 2013;55(2):130-41.
Del Brutto OH. Neurocisticercosis: actualización en diagnóstico y tratamiento. Neurología. 2005;20(8):412-8.
Shih R, Koeller K. Bacterial, fungal, and parasitic infections of the central nervous system: Radiologic-pathologic correlation and historical perspectives. RadioGraphics. 2015;35:1141-69.
Sánchez A, Monteagudo M, Lozano E, García J. Neurocisticercosis racemosa subaracnoidea gigante y ventricular: a propósito de un caso. Rev Argent Microbiol. 2015;47(3):201-5.
Teerasukjinda O, Wongjittraporn S, Tongma C, Chung H. Asymptomatic giant intraventricular cysticercosis: A Case Report. Hawaii J Med Public Health. 2016;75(7):187-9.
Matushita H, Campos F, Dante D, Jacobsen M. Hydrocephalus in neurocysticercosis. Childs Nerv Syst. 2011;27(10):1709-21.
Del Brutto OH. Neurocysticercosis. The Neurohospitalist. 2014;4(4):205-12.
Del Brutto OH. Neurocysticercosis: A Review. Scientific World J. 2012;2012:1-8. https://doi.org/10.1100/2012/159821.
Lucato L, Guedes M, Sato J, Bacheschi L, Machado L, Leite C. The role of conventional MR imaging sequences in the evaluation of neurocysticercosis: impact on characterization of the scolex and lesion Burden. Am J Neuroradiol. 2007;28(8):1501-4.
Delgado R, Boleaga B, Salgado P. Magnetic resonance imaging in neurocysticercosis. Top Magn Reson Imaging. 2014;23:191-8.
Lerner A, Shiroishi M, Zee C, Law M, Go J. Imaging of neurocysticercosis. Neuroimag Clin N Am. 2012;22:659-76.
Carpio A, Fleury A, Hauser WA. Neurocysticercosis Five new things. Neurol Clin Pract. 2013;3(2):118-25.
Brandao MD, Lara A, Domingues RC. MR spectroscopy of the brain. Philadelphia, PA: Lippincott Williams & Wilkins; 2004.
Raffin L, Bacheschi L, Machado L, Nóbrega J, Coelho C, Leite C. Diffusion- Weighted MR imaging of cystic lesions of neurocysticercosis. Arq Neuropsiquiatr 2001;59(4):839-42.
Santos G, Leite C, Machado L, McKinney A, Lucato L. Reduced diffusion in neurocysticercosis: Circumstances of appearance and possible natural history implications. Am J Neuroradiol. 2013;34(2):310-6.
Descargas
Publicado
Cómo citar
Número
Sección
Licencia

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial-CompartirIgual 4.0.
La Revista Colombiana de Radiología es de acceso abierto y todos sus artículos se encuentran libre y completamente disponibles en línea para todo público sin costo alguno.
Los derechos patrimoniales de autor de los textos y de las imágenes del artículo como han sido transferidos pertenecen a la Asociación Colombiana de Radiología (ACR). Por tanto para su reproducción es necesario solicitar permisos y se debe hacer referencia al artículo de la Revista Colombiana de Radiología en las presentaciones o artículos nuevos donde se incluyan.