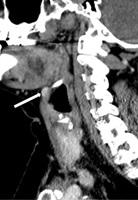
Imágenes de adenomas paratiroideos ectópicos. Una revisión de la literatura
Palabras clave:
Glándulas paratiroides, Adenoma, Tomografía computarizada por rayos XResumen
Objetivos: 1) Revisar la anatomía y epidemiología de los adenomas paratiroideos ectópicos (APE); 2) resumir el papel de las modalidades de imagen relevantes en su localización; y 3) revisar brevemente los enfoques quirúrgicos para los mismos. Métodos: Reseña literaria de artículos publicados en inglés desde 1984 hasta agosto de 2017. Resultados: El resumen de la literatura indica que la prevalencia de APE es de, aproximadamente, el 20 % en pacientes con hiperparatiroidismo primario que no han sido intervenidos quirúrgicamente, pero en pacientes reintervenidos es tan alta que alcanza el 66 %. Los APE pueden estar localizados en cualquier lugar, desde la bifurcación de la carótida hasta la ventana aortopulmonar. El ultrasonido tiene una agudeza diagnóstica limitada en su identificación, excepto para los que están localizados cerca de la glándula tiroides y al ligamento tirotímico. Requiere gran experiencia del operador. Si se comparan las técnicas de gammagrafía Sestamibi- 99mTc de fase dual, la imagen híbrida con tomografía computarizada de emisión de fotón simple (SPECT) y con tomografía computarizada (TC), la técnica SPECT/TC es superior a la gammagrafía planar o SPECT en la localización de los APE. La TC en cuatro dimensiones (4DTC) delinea con precisión las relaciones anatómicas importantes y es altamente sensible para la localización de los APE. Aunque la 4DTC requiere radiación, medio de contraste intravenoso yodado y experiencia del lector, provee buena información para detectar lesiones en varios sitios ectópicos y guiar el abordaje quirúrgico. Los APE frecuentemente requieren enfoques quirúrgicos alternativos. Se puede intentar una nueva paratiroidectomía en pacientes que han sido previamente sometidos a una exploración bilateral del cuello, por un cirujano experimentado, una vez que la lesión se localice mediante dos modalidades de imágenes. La remoción de la enfermedad no localizada requiere una exploración cuidadosa y sistemática de las localizaciones superiores e inferiores de las glándulas. Conclusión: Los APE plantean desafíos tanto para su localización como para la extirpación quirúrgica. Con el fin de obtener resultados óptimos se requiere contar con la experiencia de un alto número de pacientes y una atención multidisciplinaria.
Descargas
Referencias bibliográficas
Duke WS, Vernon HM, Terris DJ. Reoperative parathyroidectomy: Overly descended superior adenoma. Otolaryngol-Head Neck Surg. 2016;154:268-71.
Roy M, Mazeh H, Chen H, Sippel RS. Incidence and localization of ectopic parathyroid adenomas in previously unexplored patients. World J Surg. 2013;37:102-6.
Galvin L, Oldan JD, Bahl M, Eastwood JD, Sosa JA, Hoang JK. Parathyroid 4D CT and scintigraphy: What factors contribute to missed parathyroid lesions? Otolaryngol Head Neck Surg. 2016;154:847-53.
Gough I. Reoperative parathyroid surgery: The importance of ectopic location and multigland disease. ANZ J Surg. 2006;76:1048-50.
Jaskowiak N, Norton JA, Alexander HR, et al. A prospective trial evaluating a standard approach to reoperation for missed parathyroid adenoma. Ann Surg. 1996;224:308-20; discussion 320-321.
Silberfein EJ. Reoperative parathyroidectomy: Location of missed glands based on a contemporary nomenclature system. Arch Surg. 2010;145:1065.
Udelsman R. Approach to the patient with persistent or recurrent primary hyperparathyroidism. J Clin Endocrinol Metab. 2011;96:2950-8.
Noussios G, Anagnostis P, Natsis K. Ectopic parathyroid glands and their anatomical, clinical and surgical implications. Exp Clin Endocrinol Diabetes. 2012;120:604-10.
Shin JJ, Milas M, Mitchell J, Berber E, Ross L, Siperstein A. Impact of localization studies and clinical scenario in patients with hyperparathyroidism being evaluated for reoperative neck surgery. Arch Surg. 2011;146:1397-403.
Simeone DM, Sandelin K, Thompson NW. Undescended superior parathyroid gland: a potential cause of failed cervical exploration for hyperparathyroidism. Surgery. 1995;118:949-56.
Rioja P, Mateu G, Lorente-Poch L, Sancho JJ, Sitges-Serra A. Undescended parathyroid adenomas as cause of persistent hyperparathyroidism. Gland Surg. 2015;4:295-300.
Akerström G, Malmaeus J, Bergström R. Surgical anatomy of human parathyroid glands. Surgery. 1984;95:14-21.
Shen W, Düren M, Morita E, et al. Reoperation for persistent or recurrent primary hyperparathyroidism. Arch Surg. 1996;131:861-7; discussion 867-9.
Fraker DL, Doppman JL, Shawker TH, et al. Undescended parathyroid adenoma: an important etiology for failed operations for primary hyperparathyroidism. World J Surg. 1990;14:342-8.
Billingsley KG, Fraker DL, Doppman JL, et al. Localization and operative management of undescended parathyroid adenomas in patients with persistent primary hyperparathyroidism. Surgery. 1994;116:982-9.
Okuda I, Nakajima Y, Miura D, Maruno H, Kohno T, Hirata K. Diagnostic localization of ectopic parathyroid lesions: developmental consideration. Jpn J Radiol. 2010;28:707-13.
Lappas D, Noussios G, Anagnostis P, Adamidou F, Chatzigeorgiou A, Skandalakis P. Location, number and morphology of parathyroid glands: results from a large anatomical series. Anat Sci Int. 2012;87:160-4.
Wilhelm SM, Wang TS, Ruan DT, et al. The American Association of Endocrine Surgeons Guidelines for Definitive Management of Primary Hyperparathyroidism. JAMA Surg. 2016;151:959.
Zerizer I, Parsaï A, Win Z, Al-Nahhas A. Anatomical and functional localization of ectopic parathyroid adenomas: 6-year institutional experience. Nucl Med Commun. 2011;32:496-502.
Chien D, Jacene H. Imaging of Parathyroid Glands. Otolaryngol Clin North Am. 2010;43:399-415.
Yeh MW, Barraclough BM, Sidhu SB, Sywak MS, Barraclough BH, Delbridge LW. Two hundred consecutive parathyroid ultrasound studies by a single clinician: the impact of experience. Endocr Pract. 2006;12:257-63.
Haciyanli M, Lal G, Morita E, Duh Q-Y, Kebebew E, Clark OH. Accuracy of preoperative localization studies and intraoperative parathyroid hormone assay in patients with primary hyperparathyroidism and double adenoma. J Am Coll Surg. 2003;197:739-46.
Sugg SL, Krzywda EA, Demeure MJ, Wilson SD. Detection of multiple gland primary hyperparathyroidism in the era of minimally invasive parathyroidectomy. Surgery. 2004;136:1303-9.
Eslamy HK, Ziessman HA. Parathyroid scintigraphy in patients with primary hyperparathyroidism: 99mTc sestamibi SPECT and SPECT/CT. Radiographics. 2008;28:1461- 76.
Ishibashi M, Nishida H, Hiromatsu Y, Kojima K, Uchida M, Hayabuchi N. Localization of ectopic parathyroid glands using technetium-99m sestamibi imaging: comparison with magnetic resonance and computed tomographic imaging. Eur J Nucl Med. 1997;24:197-201.
Phitayakorn R, McHenry CR. Incidence and location of ectopic abnormal parathyroid glands. Am J Surg. 2006;191:418-23.
Krausz Y, Bettman L, Guralnik L, et al. Technetium-99m-MIBI SPECT/CT in primary hyperparathyroidism. World J Surg. 2006;30:76-83.
Kim SC, Kim S, Inabnet WB, Krynyckyi BR, Machac J, Kim CK. Appearance of descended superior parathyroid adenoma on SPECT parathyroid imaging. Clin Nucl Med. 2007;32:90-3.
Lavely WC, Goetze S, Friedman KP, et al. Comparison of SPECT/CT, SPECT, and planar imaging with single-and dual-phase 99mTc-Sestamibi parathyroid scintigraphy. J Nucl Med. 2007;48:1084-9.
Wong KK, Fig LM, Gross MD, Dwamena BA. Parathyroid adenoma localization with 99mTc-sestamibi SPECT/CT: a meta-analysis. Nucl Med Commun. 2015;36:363-75.
Zhen L, Li H, Liu X, Ge BH, Yan J, Yang J. The application of SPECT/CT for preoperative planning in patients with secondary hyperparathyroidism. Nucl Med Commun. 2013;34:439-44.
Serra A, Bolasco P, Satta L, Nicolosi A, Uccheddu A, Piga M. Role of SPECT/CT in the preoperative assessment of hyperparathyroid patients. Radiol Med. 2006;111:999- 1008.
Ciappuccini R, Morera J, Pascal P, et al. Dual-phase 99mTc sestamibi scintigraphy with neck and thorax SPECT/CT in primary hyperparathyroidism: a single-institution experience. Clin Nucl Med. 2012;37:223-8.
Hoang JK, Sung W, Bahl M, Phillips CD. How to perform parathyroid 4D CT: Tips and traps for technique and interpretation. Radiology. 2014;270:15-24.
Johnson NA, Tublin ME, Ogilvie JB. Parathyroid imaging: technique and role in the preoperative evaluation of primary hyperparathyroidism. AJR Am J Roentgenol. 2007;188:1706-15.
Stack BC Jr, Moore ER, Belcher RH, Spencer HJ, Bodenner DL. Hormone, Relationships of parathyroid gamma counts, and adenoma mass in minimally invasive parathyroidectomy. Otolaryngol Head Neck Surg. 2012;147:1035-40.
Ruda JM, Hollenbeak CS, Stack BC Jr. A systematic review of the diagnosis and treatment of primary hyperparathyroidism from 1995 to 2003. Otolaryngol Head Neck Surg. 2005;132:359-72.
Ho Shon IA, Yan W, Roach PJ, et al. Comparison of pinhole and SPECT 99mTc-MIBI imaging in primary hyperparathyroidism. Nucl Med Commun. 2008;29:949-55.
Tomas MB, Pugliese PV, Tronco GG, Love C, Palestro CJ, Nichols KJ. Pinhole Versus Parallel-Hole Collimators for Parathyroid Imaging: An Intraindividual Comparison. J Nucl Med Technol. 2008;36:189-194.
Bhatt PR, Klingensmith WC 3rd, Bagrosky BM, et al. Parathyroid imaging with simultaneous acquisition of 99mTc-Sestamibi and 123I: The relative merits of pinhole collimation and SPECT/CT. J Nucl Med Technol. 2015;43:275-81.
Klingensmith WC 3rd, Koo PJ, Summerlin A, et al. Parathyroid imaging: the importance of pinhole collimation with both single- and dual-tracer acquisition. J Nucl Med Technol. 2013;41:99-104.
Morón F, Delumpa A, Chetta J, Guffey D, Dunaway D. Single phase computed tomography is equivalent to dual phase method for localizing hyperfunctioning parathyroid glands in patients with primary hyperparathyroidism: a retrospective review. PeerJ. 2017;5:e3586.
Hoang JK, Reiman RE, Nguyen GB, et al. Lifetime attributable risk of cancer from radiation exposure during parathyroid imaging: Comparison of 4D CT and parathyroid scintigraphy. AJR Am J Roentgenol. 2015;204:W579-W85.
Moreno MA, Callender GG, Woodburn K, et al. Common locations of parathyroid adenomas. Ann Surg Oncol. 2011;18:1047-51.
Clark OH, Duh Q-Y, Kebebew E, eds. Atlas of endocrine surgical techniques. Philadelphia, PA: Saunders/Elsevier; 2010.
Perrier ND, Edeiken B, Nunez R, et al. A novel nomenclature to classify parathyroid adenomas. World J Surg. 2009;33:412-6.
Morris LF, Lee S, Warneke CL, et al. Fewer adverse events after reoperative parathyroidectomy associated with initial minimally invasive parathyroidectomy. Am J Surg. 2014;208:850-5.
Stack, BC, Bodenner DL, eds. Medical and surgical treatment of parathyroid diseases. Cham, Switzerland: Springer International Publishing; 2017.
Irvin GL, Molinari AS, Figueroa C, Carneiro DM. Improved success rate in reoperative parathyroidectomy with intraoperative PTH assay. Ann Surg. 1999;229(6):874-8; discussion 878-9.
McIntyre CJ, Allen JL, Constantinides VA, Jackson JE, Tolley NS, Palazzo FF. Patterns of disease in patients at a tertiary referral centre requiring reoperative parathyroidectomy. Ann R Coll Surg Engl. 2015;97:598-602.
Publicado
Cómo citar
Número
Sección
Licencia

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial-CompartirIgual 4.0.
La Revista Colombiana de Radiología es de acceso abierto y todos sus artículos se encuentran libre y completamente disponibles en línea para todo público sin costo alguno.
Los derechos patrimoniales de autor de los textos y de las imágenes del artículo como han sido transferidos pertenecen a la Asociación Colombiana de Radiología (ACR). Por tanto para su reproducción es necesario solicitar permisos y se debe hacer referencia al artículo de la Revista Colombiana de Radiología en las presentaciones o artículos nuevos donde se incluyan.