Testicular Lymphoma: Case Series. Findings in Ultrasound Mode B, Color and Spectral Doppler
DOI:
https://doi.org/10.53903/01212095.22Keywords:
Testicular neoplasm, Lymphoma, Ultrasonography, DopplerAbstract
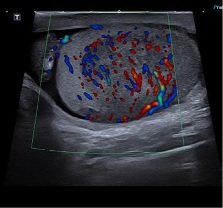
Primary testicular lymphoma is an uncommon and aggressive neoplasm, with a mean age of diagnosis between 66 and 68 years, corresponding to the most common primary testicular neoplasm in those over 60 years of age and with bilateral involvement. Secondary testicular lymphoma is much more common and includes extranodal relapse after chemotherapy and primary manifestations of unknown systemic disease. The imaging characteristics of testicular lymphoma reflect a non-destructive infiltrative pattern seen in histopathological analyzes, which is reflected in its ultrasound manifestations. We present a series of cases with a confirmed diagnosis of testicular lymphoma to describe the most frequent findings in B-mode ultrasonography, color and spectral Doppler.
Downloads
References
Moreno CC, Small WC, Camacho JC, Master V, Kokabi N, Lewis M, et al. Testicular tumors: What radiologists need to know—differential diagnosis, staging, and management. Radiographics. 2015;35(2):400-15.
Moorjani V, Mashankar A, Goel S, Khandelwal K, Patange V, Merchant N. Sonographic appearance of primary testicular lymphoma. Am J Roentgenol. 1991;157(6):1225-6.
Lantz AG, Power N, Hutton B, Gupta R. Malignant lymphoma of the testis: A study of 12 cases. J Can Urol Assoc. 2009;3(5):393-8.
Bertolotto M, Lorenzo D, Mustafá S, Vikram D. Grayscale and color doppler features of testicular lymphoma. J Ultrasound Med. 2015;34(6):1139-45.
Zicherman JM, Weissman D, Gribbin C, Epstein R. Best cases from the AFIP: Primary diffuse large B-cell lymphoma of the epididymis and testis. Radiographics. 2005;25(1):243-8.
Ishigami K, Yousef-Zahra DM, Abu-Yousef MM. Enlargement and hypervascularity of both the epididymis and testis do not exclude involvement with lymphoma or leukemia. J Clin Ultrasound. 2004;32(7):365-9.
Dalal V, Kaur M, Siraj F, Singh A, Bansal A. Primary testicular lymphoma with solitary cutaneous nodule as the initial presentation. J Can Urol Assoc. 2015;9(9-10):E744-7.
Cheah CY, Wirth A, Seymour JF. Review article primary testicular lymphoma. Blood. 2018;123(4):486-94.
Mazzu D, Jeffrey RB, Ralls PW. Lymphoma and leukemia involving the testicles: Findings on gray - scale and color Doppler sonography. Am J Roentgenol. 1995;164(3):645-7.
Shahab N, Doll DC. Testicular lymphoma. Semin Oncol. 1999;26(3):259-69.
Tweed CS, Peck RJ. A sonographic appearance of testicular lymphoma. Clin Radiol. 1991;43(5):341-2.
Bhatt S, Dogra V. Role of US in testicular and scrotal trauma. RadioGraphics. 2008;28:1617-29.
Deurdulian C, Mittelstaedt C, et al. US of Acute scrotal trauma: Optimal technique, imaging findings, and management. RadioGraphics. 2007;27(2):357-69.
Avery L, Scheinfeld M. imaging of Penile and scrotal emergencies. RadioGraphics. 2013;33:721-40.
Woodward P, et al. From the Archives of the AFIP. RadioGraphics. 2002;22(1):189-216.
Marko J, et al. Testicular seminoma and its mimics. RadioGraphics. 2017;37:1085-98.
Downloads
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
La Revista Colombiana de Radiología es de acceso abierto y todos sus artículos se encuentran libre y completamente disponibles en línea para todo público sin costo alguno.
Los derechos patrimoniales de autor de los textos y de las imágenes del artículo como han sido transferidos pertenecen a la Asociación Colombiana de Radiología (ACR). Por tanto para su reproducción es necesario solicitar permisos y se debe hacer referencia al artículo de la Revista Colombiana de Radiología en las presentaciones o artículos nuevos donde se incluyan.