Multifocal Brown Tumor as A Manifestation Of Primary Parathyroid Carcinoma. A Case Report
DOI:
https://doi.org/10.53903/01212095.50Keywords:
Osteitis fibrosa cystica, Parathyroid neoplasms, Primary hyperparathyroidism, RadiographyAbstract
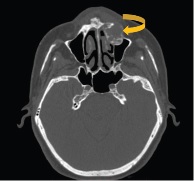
Parathyroid carcinoma is an exceptional cause of primary hyperparathyroidism. Brown tumors develop as skeletal manifestations of primary hyperparathyroidism in the context of advanced disease. They are highly vascular, lytic bone lesions with a reparative cellular process instead of a neoplastic process. They can be identified in the secondary forms of the disease, however, they are more frequent in primary hyperparathyroidism. We present a case of multiple brown tumors secondary to parathyroid carcinoma. The initial manifestation of primary hyperparathyroidism was a pathological fracture secondary to brown tumor associated with hypercalcemia and elevated levels of parathyroid hormone (PTH), which is rare due to the fact that in recent decades the incorporation of serum calcium in routine laboratory tests detects this disease in asymptomatic or minimally symptomatic stages. Ultrasound detected a vascularized solid lesion in the anatomical site of the left lower parathyroid and nephrocalcinosis. The lesion was surgically resected in the left hemicolumn and the biopsy reported parathyroid carcinoma. Brown tumors are non-neoplastic lesions that do not have malignant potential and are therefore considered repairing granulomas.
Downloads
References
Xie C, Tsakok M, Taylor N, Partington K. Imaging of brown tumours: a pictorial review. Insights Imag. 2019;10(1). doi: 10.1186/s13244-019-0757-z.
Arias W, Ayala A, Pacheco F, Barzallo D. Tumor pardo multifocal como manifestación del hiperparatiroidismo primario por adenoma paratiroideo asociado a carcinoma papilar de tiroides. Rev Chil Cir. 2014;66(6):592-8. doi: 10.4067/s0718- 40262014000600014.
Madkhali T, Alhefdhi A, Chen H, Elfenbein D. Primary hyperparathyroidism. Turkish J Surg. 2016;32(1):58-66. doi: 10.5152/ucd.2015.3032.
Alfawareh M, Halawani M, Attia W, Almusrea K. Brown tumor of the cervical spines: A case report with literature review. Asian Spine J. 2015;9(1):110. doi: 10.4184/ asj.2015.9.1.110.
Kwon J, Kim E, Lee H, Moon H, Kwak J. Neck ultrasonography as preoperative localization of primary hyperparathyroidism with an additional role of detecting thyroid malignancy. European J Radiol. 2013;82(1):e17-e21. 10.1016/j.ejrad.2012.08.003.
McDonald D, Parman L, Speights V. Primary hyperparathyroidism due to parathyroid adenoma. RadioGraphics. 2005;25(3):829-34. doi: 10.1148/rg.253045042.
Mora-Escudero I, Gato-Díez A, Blázquez-Cabrera J, Lozano-Setien E, García-de-la- Torre J. Tumores pardos pretibiales como manifestación inicial de un hiperparatiroidismo primario. Rev Clín Española. 2012;212(3):e15-e18. doi:10.1016/j.rce.2011.07.014.
Herrera A, Aranda P, Díaz J. Cáncer de paratiroides: revisión de literatura. Rev Española Enfermed Metaból Óseas. 2007;16(6):124-9. doi:10.1016/s1132-8460(07)73511-0.
Morán L, Moeinvaziri M, Fernández A, Sánchez R. Multiple brown tumors mistaken for bone metastases. Computed tomography imaging findings. Egyptian J Radiol Nucl Med. 2016;47(2):537-41. doi: 10.1016/j.ejrnm.2016.03.001.
Rocha AL, Suazo LC, González PM, Lee ChK, Rossel DG. Hiperparatiroidismo primario y cáncer de paratiroides: Caso clínico. Rev Chil Cirugía. 2010;62(5). doi: 10.4067/s0718-40262010000500016.
Jakubowski J, Vélez I, McClure S. Brown tumor as a result of hyperparathyroidism in an end-stage renal disease patient. Case Reports Radiol. 2011;2011:1-3. doi: 10.1155/2011/415476.
Parra Ramírez P, Lecumberri Santamaría B, Álvarez Escolá C, Pallardo Sánchez L. Hiperparatiroidismo primario con osteítis fibrosa quística simulando una neoplasia ósea maligna. Endocrinol Nutric. 2013;60(2):96-8. doi: 10.1016/j.endonu.2012.02.012.
Ferraro V, Sgaramella LI, Di Meo G, et al. Current concepts in parathyroid carcinoma: a single Centre experience. BMC Endocr Disord. 2019;19(46). https://doi.org/10.1186/s12902-019-0368-1.
Fernandes J, Paiva C, Correia R, Polónia J, Moreira da Costa A. Parathyroid carcinoma: From a case report to a review of the literature. Inter J Surg Case Reports. 2018;42:214-7. doi: 10.1016/j.ijscr.2017.11.030.
Rosai JDR, Carcangiu ML, Frable WJ, Tallini G. Tumors of the thyroid and parathyroid glands. AFIP Atlas of Tumor Pathology. Silver Spring, Maryland: ARP Press; 2014.
Betea D, Bradwell A, Harvey T, Mead G, Schmidt-Gayk H, Ghaye B et al. Hormonal and biochemical normalization and tumor shrinkage induced by anti-parathyroid hormone immunotherapy in a patient with metastatic parathyroid carcinoma. J Clin Endocrinol Metabolism. 2004;89(7):3413-20. doi: 10.1210/jc.2003-031911.
Erickson L, Mete O. Immunohistochemistry in diagnostic parathyroid pathology. Endocrine Pathol. 2018;29(2):113-29. doi: 10.1007/s12022-018-9527-6.
Shi C, Guan H, Qi W, Ji J, Wu J, Yan F et al. Intrathyroidal parathyroid adenoma: Diagnostic pitfalls on fine-needle aspiration: Two case reports and literature review. Diagnostic Cytopathol. 2016;44(11):921-5. doi: 10.1002/dc.23528.
Wong Y, Sharifah N, Tan G, Gill A, Ali S. Intrathyroidal oxyphilic parathyroid carcinoma: A potential diagnostic caveat in cytology? Diagnostic Cytopathol. 2016;44(8):688- 92. doi: 10.1002/dc.23493.
Shane E. Parathyroid carcinoma. J Clin Endocrinol Metabolism. 2001;86(2):485-93. doi: 10.1210/jcem.86.2.7207.
García J, Álvarez Moro F, Bassa P, Soler M, Llinares E, Riera E. Detección de tumores pardos por hiperparatiroidismo secundario mediante PET/TC con 11C-colina. Rev Española Med Nuclear Imagen Molecular. 2016;35(3):209-10. doi: 10.1016/j. remn.2015.07.009.
Insogna K. Primary hyperparathyroidism. New Engl J Med. 2018;379(11):1050-9. doi: 10.1056/nejmcp1714213.
Piciucchi S, Barone D, Gavelli G, Dubini A, Oboldi D, Matteuci F. Primary hyperparathyroidism: imaging to pathology. J Clin Imag Sci. 2012;2:59. doi: 10.4103/2156- 7514.102053.
Park S, Kong G, Kwon Y, Park J. Pathologic fracture of the femur in brown tumor induced in parathyroid carcinoma: A Case Report. Hip Pelvis. 2016;28(3):173. doi: 10.5371/hp.2016.28.3.173.
Park Y, Yoon T, Park K, Ko J. Subchondral bone restoration of supra-acetabular brown tumor secondary to parathyroid carcinoma: A Case Report. Hip Pelvis. 2018;30(2):120. doi: 10.5371/hp.2018.30.2.120.
Marcocci C, Cetani F. Primary hyperparathyroidism. New Eng J Med. 2011;365(25):2389-97. doi: 10.1056/nejmcp1106636.
Radulescu D, Chis B, Donca V, Münteanu V. Brown tumors of the femur and pelvis secondary to a parathyroid carcinoma: Report of one case. Rev Méd Chile. 2014;142(7):919-23. doi: 10.4067/s0034-98872014000700014.
Kim Y. Parathyroid carcinoma with lung metastasis in a thirteen-year-old girl. J Korean Surg Society. 2012;82(6):385. doi: 10.4174/jkss.2012.82.6.385.
Fortson J, Su R, Patel V, Lawrence G. Parathyroid carcinoma presenting with pathologic fracture: Case report and review of the literature. Head Neck. 2015;37(11):E139-E141. doi: 10.1002/hed.23965
Downloads
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
La Revista Colombiana de Radiología es de acceso abierto y todos sus artículos se encuentran libre y completamente disponibles en línea para todo público sin costo alguno.
Los derechos patrimoniales de autor de los textos y de las imágenes del artículo como han sido transferidos pertenecen a la Asociación Colombiana de Radiología (ACR). Por tanto para su reproducción es necesario solicitar permisos y se debe hacer referencia al artículo de la Revista Colombiana de Radiología en las presentaciones o artículos nuevos donde se incluyan.